By HANNAH RECHT
Kaiser Health News, courtesy Daily Montanan
Nearly 6 million Americans have taken Paxlovid for free, courtesy of
the federal government. The Pfizer pill has helped prevent many people
infected with COVID-19 from being hospitalized or dying, and it may even reduce the risk
of developing long COVID. But the government plans to stop footing the
bill within months, and millions of people who are at the highest risk
of severe illness and are least able to afford the drug — the uninsured
and seniors — may have to pay the full price.
And that means fewer people will get the potentially lifesaving treatments, experts said.
“I think the numbers will go way down,” said Jill Rosenthal, director
of public health policy at the Center for American Progress, a
left-leaning think tank. A bill for several hundred dollars or more
would lead many people to decide the medication isn’t worth the price,
she said.
In response to the unprecedented public health crisis caused by
COVID, the federal government spent billions of dollars on developing
new vaccines and treatments, to swift success: Less than a year after
the pandemic was declared, medical workers got their first vaccines. But
as many people have refused the shots and stopped wearing masks, the
virus still rages and mutates. In 2022 alone, 250,000 Americans have died from COVID, more than from strokes or diabetes.
But soon the Department of Health and Human Services will stop
supplying COVID treatments, and pharmacies will purchase and bill for
them the same way they do for antibiotic pills or asthma inhalers.
Paxlovid is expected to hit the private market in mid-2023, according to
HHS plans shared in an October meeting with state health officials and
clinicians. Merck’s Lagevrio, a less-effective COVID treatment pill, and
AstraZeneca’s Evusheld, a preventive therapy for the immunocompromised,
are on track to be commercialized sooner, sometime in the winter.
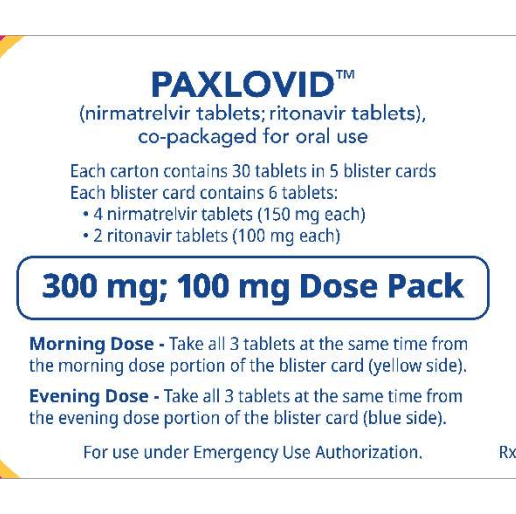
The U.S. government has so far purchased 20 million courses
of Paxlovid, priced at about $530 each, a discount for buying in bulk
that Pfizer CEO Albert Bourla called “really very attractive” to the
federal government in a July earnings call. The drug will cost far more
on the private market, although in a statement to KHN, Pfizer declined
to share the planned price. The government will also stop paying for the
company’s COVID vaccine next year — those shots will quadruple in price, from the discount rate the government pays of $30 to about $120.
Bourla told investors in November that he expects the move will make
Paxlovid and its COVID vaccine “a multibillion-dollars franchise.”
Nearly 9 in 10 people dying from the virus now are 65 or older. Yet federal law restricts Medicare Part D — the prescription drug program that covers nearly 50 million seniors
— from covering the COVID treatment pills. The medications are meant
for those most at risk of serious illness, including seniors.
Paxlovid and the other treatments are currently available under an
emergency use authorization from the FDA, a fast-track review used in
extraordinary situations. Although Pfizer applied for full approval
in June, the process can take anywhere from several months to years.
And Medicare Part D can’t cover any medications without that full stamp
of approval.
Paying out-of-pocket would be “a substantial barrier” for seniors on
Medicare — the very people who would benefit most from the drug, wrote federal health experts.
“From a public health perspective, and even from a health care
capacity and cost perspective, it would just defy reason to not continue
to make these drugs readily available,” said Dr. Larry Madoff, medical
director of Massachusetts’ Bureau of Infectious Disease and Laboratory
Sciences. He’s hopeful that the federal health agency will find a way to
set aside unused doses for seniors and people without insurance.
In mid-November, the White House requested that Congress approve an
additional $2.5 billion for COVID therapeutics and vaccines to make sure
people can afford the medications when they’re no longer free. But
there’s little hope it will be approved — the Senate voted that same day to end the public health emergency and denied similar requests in recent months.
Many Americans have already faced hurdles just getting a prescription for COVID treatment. Although the federal government doesn’t track who’s gotten the drug, a Centers for Disease Control and Prevention study
using data from 30 medical centers found that Black and Hispanic
patients with COVID were much less likely to receive Paxlovid than white
patients. (Hispanic people can be of any race or combination of races.)
And when the government is no longer picking up the tab, experts
predict that these gaps by race, income, and geography will widen.
People in Northeastern states used the drug far more often than those
in the rest of the country, according to a Kaiser Health News analysis
of Paxlovid use in September and October. But it wasn’t because people
in the region were getting sick from COVID at much higher rates —
instead, many of those states offered better access to health care to begin with and created special programs to get Paxlovid to their residents.
About 10 mostly Democratic states and several large counties in the
Northeast and elsewhere created free “test-to-treat” programs that allow
their residents to get an immediate doctor visit and prescription for
treatment after testing positive for COVID. In Massachusetts, more than
20,000 residents have used the state’s video and phone hotline,
which is available seven days a week in 13 languages. Massachusetts,
which has the highest insurance rate in the country and relatively low
travel times to pharmacies, had the second-highest Paxlovid usage rate
among states this fall.
States with higher COVID death rates, like Florida and Kentucky,
where residents must travel farther for health care and are more likely
to be uninsured, used the drug less often. Without no-cost test-to-treat
options, residents have struggled to get prescriptions even though the drug itself is still free.
“If you look at access to medications for people who are uninsured, I
think that there’s no question that will widen those disparities,”
Rosenthal said.
People who get insurance through their jobs could face high copays at
the register, too, just as they do for insulin and other expensive or
brand-name drugs.
Most private insurance companies will end up covering COVID
therapeutics to some extent, said Sabrina Corlette, a research professor
at Georgetown University’s Center on Health Insurance Reforms. After
all, the pills are cheaper than a hospital stay. But for most people who
get insurance through their jobs, there are “really no rules at all,”
she said. Some insurers could take months to add the drugs to their
plans or decide not to pay for them.
And the additional cost means many people will go without the medication.
“We know from lots of research that when people face cost sharing for
these drugs that they need to take, they will often forgo or cut back,”
Corlette said.
One group doesn’t need to worry about sticker shock. Medicaid, the
public insurance program for low-income adults and children, will cover
the treatments in full until at least early 2024.
HHS officials could set aside any leftover taxpayer-funded medication
for people who can’t afford to pay the full cost, but they haven’t
shared any concrete plans to do so. The government purchased 20 million
courses of Paxlovid and 3 million of Lagevrio. Fewer than a third have
been used, and usage has fallen in recent months, according to KHN’s
analysis of the data from HHS.
Sixty percent of the government’s supply of Evusheld is also still available, although the COVID prevention therapy is less effective against new strains of the virus. The health department in one state, New Mexico, has recommended against using it.
HHS did not make officials available for an interview or answer written questions about the commercialization plans.
The government created a potential workaround when they moved
bebtelovimab, another COVID treatment, to the private market this
summer. It now retails for $2,100 per patient. The agency set aside the
remaining 60,000 government-purchased doses that hospitals could use to
treat uninsured patients in a convoluted dose-replacement process. But it’s hard to tell how well that setup would work for Paxlovid: Bebtelovimab was already much less popular, and the FDA halted its use on Nov. 30 because it’s less effective against current strains of the virus.
Federal officials and insurance companies would have good reason to
make sure patients can continue to afford covid drugs: They’re far
cheaper than if patients land in the emergency room.
“The medications are so worthwhile,” said Madoff, the Massachusetts
health official. “They’re not expensive in the grand scheme of health
care costs.”
KHN
(Kaiser Health News) is a national newsroom that produces in-depth
journalism about health issues. Together with Policy Analysis and
Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
